by Bobby Anderson, RN, Staff Writer
It was the morning of January 10, 2018 and Kim Shannon, RN, woke up to start another day.
As a clinical instructor for Moore Norman Technology Center, Shannon would be checking on students at clinical sites across the metro.
Only if she could get the bathroom door knob open.
“I couldn’t make it turn,” Shannon remembers. “I remember getting really upset that my arm was so weak.”
That doorknob never turned as Shannon went through the initial phases of a massive stroke. But little did she know her husband’s call to 911 would set in motion a finely-tuned process that would save her life.
“I’m kind of an anomaly,” Shannon said one year later. “Most people that have the kind of stroke I had are dead or they’re not able to communicate in any way.
“God just wasn’t ready for me. Everybody was in place at the right time.”
That phone call started an EMSSTAT ambulance to her location East of Hwy 9 in Norman. Paramedics quickly realized the situation and radioed ahead a Code Stroke to Norman Regional Hospital’s Porter Campus.
“They didn’t waste any time,” Shannon said. “The paramedic started an IV while we were driving and they were driving fast. She told me ‘we’re going lights and sirens. Don’t be scared. We just need to get you there quickly.’”
TIME IS BRAIN
According to the American Heart Association journal, Stroke, every minute in which a large vessel ischemic stroke is untreated, the average patient loses 1.9 million neurons, 13.8 billion synapses, and seven miles of axonal fibers. Each hour in which treatment fails to occur, the brain loses as many neuron as it does in almost 3.6 years of normal aging.
That’s why ER staff were waiting at the door.
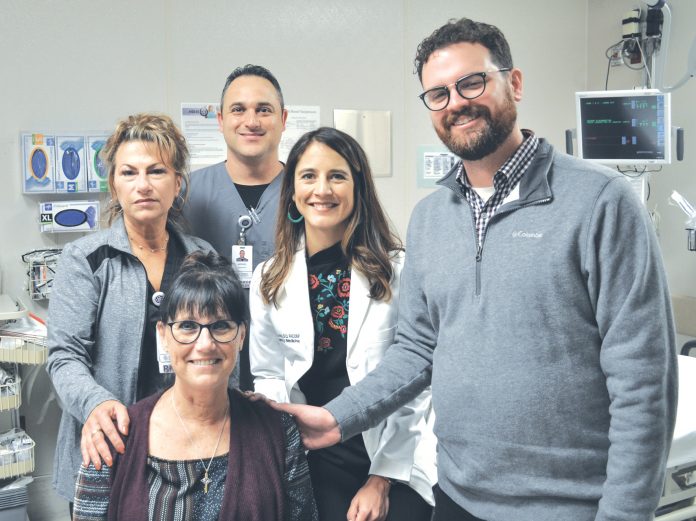
As luck would have it Carla Lewis, RN, was there, too.
“She and I went to nursing school together,” Shannon smiled. “I had known her forever. That made me comfortable right away. I knew Carla was going to take good care of me.”
ER Dr. Michael Porter was there, too, assessing Shannon and explaining if she had a blood clot then tissue plasminogen activator (tPA) would be indicated to restore blood flow.
Shannon was sent straight back for a CT scan of her head.
“As I was still rolling out of the machine Dr. Porter was there with a resident and two syringes,” Shannon remembered. “He said ‘you have two clots.’ They gave (tPA) to me right then. It was that quick. Everything happened right because my brain was already 50 minutes with no oxygen.”
Shannon received tPA within 16 minutes of arrival. National stroke guidelines call for administration within 60 minutes.
Thirty minutes later, Shannon started saying words, moving her right thumb and wiggling toes as one clot dissolved.
Another ambulance rushed her to OU Medical Center for a thrombectomy to be performed by Dr. Bradley Bohnstedt.
The second clot was retrieved within four-and-a-half hours of onset.
Even on a day of so much trauma, Shannon remembers so much detail.
There was Carla’s peach scrubs, signature messy bun hairdo and how beautiful she looked.
“I remember his face,” Shannon said of Dr. Porter. “He was kind and he did everything he was supposed to do and it worked.”
She remembers nurse Lisa at OU Medical Center. There was Barney in ICU, Kate the stroke director and Heather.
And then there was Dr. Bohnstedt.
“I remember (in the cath lab) him asking for a No. 8 and getting really frustrated when they couldn’t find one,” Shannon said. “I remember thinking ‘somebody give him the damn No. 8.’”
Before the stroke, Shannon was an OR nurse at Norman Regional before starting the Surgical Technology program at Moore Norman Technology Center in the late 1990s.
She tried to go back to work. One month later she experienced a total reactivation of the stroke site.
“When I have too much stress or use my brain too much a portion of my brain shuts down to protect itself,” said Shannon, who says she’s lost much attention to detail. “It happens when I get sick or during busy times. It’s frightening, nonetheless. I’m a little bit afraid that maybe this one will stay or it’s another stroke.”
“I know I’m probably never going to be 100 percent and I know I’m not going to be able to work as a nurse and I’m OK with that. I’ve made my peace with that,” Shannon continued. “But I’m able to live a full life – a good life – and enjoy my kids and grandkids.”
It’s outcomes like Shannon’s that drive Courtney Stark, RN, who oversees stroke care at Norman Regional’s three campuses.
“I think we’ve done amazing,” Stark said of her program. “I’ve been very impressed. Some of the hats some of the people in our committee wear are multiple. Other facilities they have a community education person, someone who does just their data, a coordinator, a manager – they have so many people that can help run their program.
“I think the fact we have fewer of these, we’re smaller and what we’re doing just proves we’re doing it for the patient. It would be easy to say we don’t have the resources.”
Shannon is happy.
“It worked perfectly and I hope that it works that way for everybody,” she said. “I know things don’t always go right – it’s the wrong time of day or there’s three people in front of you – but it worked for me.”
Your future starts with us
RN Manager (night shift)
The Children’s Center Rehabilitation Hospital is a private, nonprofit hospital offering 24-hour medical care, comprehensive rehabilitative therapies, respiratory care, and special education.
· Competitive salaries · Excellent benefits · Great work environment · Professional growth · Wellness program
The Children’s Center Rehabilitation Hospital
Learn more and apply: miracleshappenhere.org
EOE