Geriatrics, infectious disease, nursing and public health experts at the University of Oklahoma Health Sciences Center are offering training to nursing home providers across Oklahoma on how to best keep their residents safe and engaged as the COVID-19 pandemic continues.
In Oklahoma, 40% of all deaths due to COVID-19 are among nursing home residents, yet they account for less than 1% of the state’s population. At the same time, there is a rise in infections among people ages 18 to 35, which tends to be the age of nursing home staff, who may unknowingly bring the virus into the facility. Those factors underscore the necessity of training and creating best practices concerning COVID-19, said geriatrician Lee Jennings, M.D., faculty member in the OU College of Medicine. (story continues below)
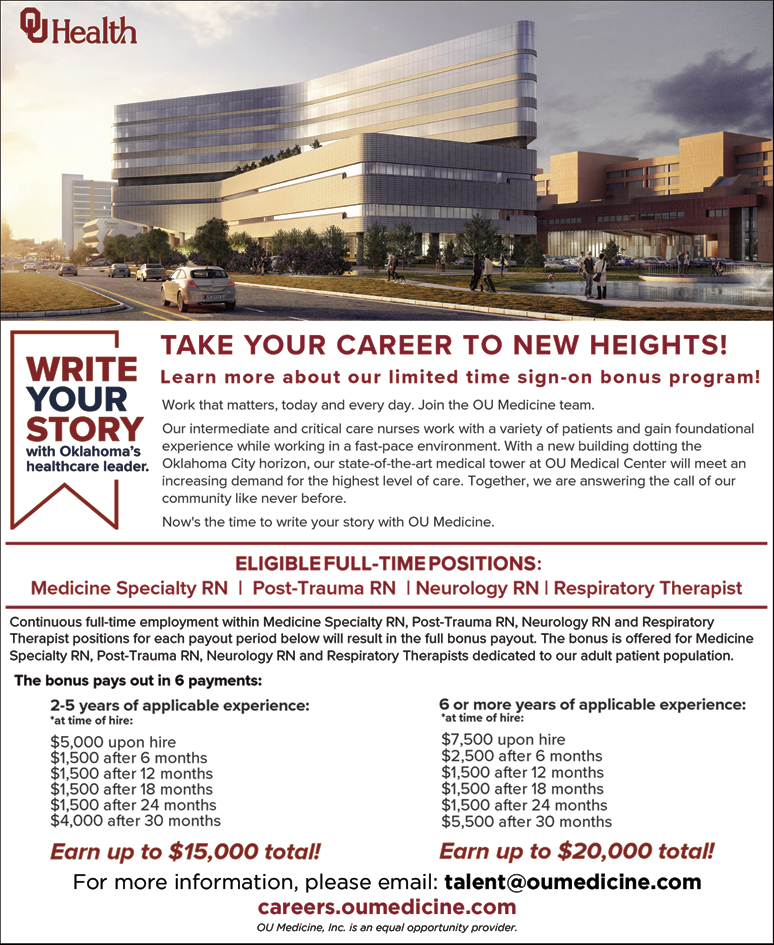
WRITE YOUR STORY with Oklahoma’s healthcare leader.
Learn more about our limited time sign-on bonus program!
Work that matters, today and every day. Join the OU Medicine team.
Our intermediate and critical care nurses work with a variety of patients and gain foundational experience while working in a fast-pace environment.
With a new building dotting the Oklahoma City horizon, our state-of-the-art medical tower at OU Medical Center will meet an increasing demand for the highest level of care.
Together, we are answering the call of our community like never before. Now’s the time to write your story with OU Medicine.
ELIGIBLE FULL-TIME POSITIONS:
Medicine Specialty RN | Post-Trauma RN | Neurology RN | Respiratory Therapist
Continuous full-time employment within Medicine Specialty RN, Post-Trauma RN, Neurology RN and Respiratory
Therapist positions for each payout period below will result in the full bonus payout. The bonus is offered for Medicine
Specialty RN, Post-Trauma RN, Neurology RN and Respiratory Therapists dedicated to our adult patient population.
The bonus pays out in 6 payments:
2-5 years of applicable experience:
*at time of hire:
$5,000 upon hire
$1,500 after 6 months
$1,500 after 12 months
$1,500 after 18 months
$1,500 after 24 months
$4,000 after 30 months
Earn up to $15,000 total!
6 or more years of applicable experience:
*at time of hire:
$7,500 upon hire
$2,500 after 6 months
$1,500 after 12 months
$1,500 after 18 months
$1,500 after 24 months
$5,500 after 30 months
Earn up to $20,000 total!
For more information, please email: [email protected]
careers.oumedicine.com
OU Medicine, Inc. is an equal opportunity employer.
“Older adults who live in nursing homes tend to be frail and in poor health, which puts them at much higher risk for bad outcomes or death if they contract COVID-19,” Jennings said. “We want to train and support nursing home providers so they can prevent COVID-19 infections and be prepared for how to care for residents who do become infected. Nursing homes also need to be prepared to respond to changing regulations and have best practices around personal protective equipment, and screening and testing staff members, among other considerations.”
The OU Health Sciences Center is uniquely positioned to offer this training because it has existing relationships with nursing homes through the Oklahoma Dementia Care Network. The value of these partnerships is evident as the COVID-19 training launches, Jennings said.
The training is being funded by the federal Agency for Healthcare Research and Quality through a program called Project ECHO (Extension for Community Healthcare Outcomes). Based at the University of New Mexico, Project ECHO is a national model that allows partners like the OU Health Sciences Center to access the most current medical information and best practices for nursing home providers during COVID-19. Project ECHO addresses many other health issues by partnering with academic medical centers to train primary care physicians in underserved and remote areas to become experts in subspecialty care.
The training, which is being offered to all Oklahoma nursing homes, consists of a 16-week boot camp for managing COVID-19 and related quality improvement steps, plus weekly “office hours” for a year. All sessions will be conducted virtually on Zoom. Each participating nursing home receives up to $6,000 to use as they need, Jennings said. In addition to specialists from the OU Health Sciences Center, national quality improvement experts from the Institute for Healthcare Improvement will take part in each session. Other collaborators include the Oklahoma State Department of Health, the Oklahoma Foundation for Medical Quality, and Telligen, the quality improvement organization designated for Oklahoma by the U.S. Centers for Medicare & Medicaid Services.
In addition to training and mentoring nursing home providers on issues specific to the virus, the sessions will address social isolation and continuing mobility for residents during the pandemic, Jennings said.
“While it has been necessary for nursing homes to limit visitation, that has been really hard on residents and families. There are spouses who have spent every day of their adult lives together and now can’t see one another. The toll it is taking is heartbreaking. There are similar situations with their children, grandchildren and other family members,” she said. “We want to promote guidelines for visitation when that becomes possible, perhaps visiting outside with family members wearing personal protective equipment. For now, we can use technology for virtual visits, and we need to make sure everyone involved knows how to best do that.”
Nursing home staff should also help residents and families talk about their loved one’s wishes should they become infected and very sick with COVID-19, Jennings said. “Best practices for advance care planning are important,” she said. “It’s vital that nursing home staff know what your loved one would want in that situation – do they want to go to the hospital, and what are their wishes for treatment if they do go the hospital? The impact of COVID-19 has pushed those conversations to the forefront in nursing homes, and we can help.”
After COVID-19 training is finished, the same network will be helpful for nursing homes going forward as other issues develop, such as making COVID-19 vaccines available, or additional topics that are especially relevant to nursing homes, Jennings said.
“This new network is a nice opportunity to provide nursing homes with the latest information and quality improvement tools on an ongoing basis,” she said. “It’s also a valuable tool for nursing home providers to reach out to their peers in other facilities and ask them what does and doesn’t work. No one knows better what the challenges are than the people who work in nursing homes. Ultimately, we all want to take the very best care of older adults that we can.”
Nursing homes can sign up to participate by emailing [email protected], calling (405) 271-8166 or visiting dcn.ouhsc.edu.













