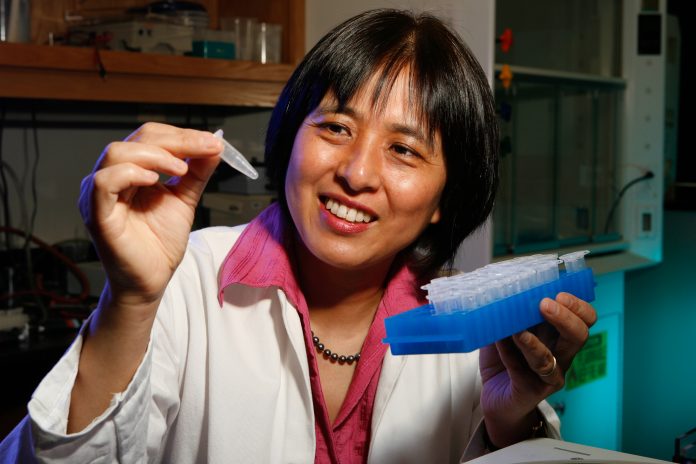
The National Institute of Allergy and Infectious Diseases has awarded Oklahoma Medical Research Foundation scientist Xiao-Hong Sun, Ph.D., a five-year, $2.76 million grant to investigate a recently discovered immune cell involved in asthma.
The role of the new cell, called an innate lymphoid cell, is to protect the body from parasitic infection. However, when too much of this cell type is present, it seems to result in asthma.
“These cells were previously thought to be made only in bone marrow,” said Sun, who holds the Lew and Myra Ward Chair in Biomedical Research at OMRF. “We discovered that they are also made in the thymus, which brings up some interesting connections to asthma.”
The thymus, which sits on top of the heart, is a major site for the creation of T cells, a type of specialized white blood cell that plays a central role in immunity. During childhood and through puberty, the thymus generates a lifetime supply of T cells—enough to carry through adulthood. When the supply of T cells is adequate, the thymus has done its job and begins to shrink.
Sun postulates that innate lymphoid cells are also present in the thymus and might explain why children have higher rates of asthma than adults.
“Since kids have a very active thymus when they’re born and up to puberty, they’re more likely to have a large number of innate lymphoid cells coming from the thymus along with the T cells,” said Sun. “This is also the stage of life where many kids tend to develop asthma. People often say they ‘grow out” of asthma as they get older, so maybe it’s linked to this later decrease in thymus function. That’s what we hope to find out with this grant.”
According to the Centers for Disease Control and Prevention, 7.7 percent of people in the United States suffer from asthma. The highest rates of asthma occur in the 5-14 age group at 10.3 percent and decline over time, reaching a low point of 6.9 percent in Americans over the age of 65.
“We don’t yet know the significance of this finding, but if we determine this hypothesis to be true, it would have great clinical relevance,” she said. “Perhaps the thymus is where we need to look for ways to control asthma in children. That’s what we hope to learn.”
The grant will also allow Sun and her lab to further investigate whether the innate lymphoid cells produced in the thymus differ from the ones made in the bone marrow.
Sun said their discovery of innate lymphoid cells in the thymus came about by accident through study of a particular mouse model in their lab—a model they’ve used for more than two decades to study T cell development.
“This research builds on our experience and what we have been working on the past 25 years, so it puts us in a unique position to do this work,” she said. “I am very excited to see how this cell is controlled and hope we can learn what happens in the thymus and how it might be linked to asthma. It really fits really well with the overall research of this lab and comes back to what started this lab in the first place.”