Courtney Elliott’s heart stopped beating on a procedure room table on February 2, 2022, three weeks after delivering her baby. Her condition was caused by a massive blood clot, a complication from a COVID-19 infection at 36 weeks pregnant.
It took more than 100 Mercy co-workers from 21 hospital departments working together over nine weeks to save Elliott’s life not once, not twice, but three times.
Her story began on New Year’s Day 2022, when an at-home COVID-19 test confirmed the body aches, exhaustion and shortness of breath she was experiencing weren’t simply the result of late-stage pregnancy.
Elliott initially monitored minor symptoms at home. A week later, her breathing had become so labored, her OB/GYN, Dr. Jennifer Strebel, determined the safest option was to deliver as soon as possible.
“She was having a really hard time breathing,” said Dr. Strebel. “I consulted with her maternal-fetal medicine specialist, and together we decided the baby was full term. If we could just deliver the baby, her uterus would decompress and allow her lungs to work more effectively.”
Dr. Strebel delivered a heathy 7-pound, 7-ounce baby girl January 12 during an emergency cesarean section at Mercy. It was an otherwise joyous occasion, and Elliott’s condition improved immediately.
“Her shortness of breath was gone, she could breathe and walk on her own and she continued to improve over the next five days until we felt it was safe for her to go home,” Strebel said.
On January 16, Elliott and her husband took their daughter home to meet her 3-year-old brother and extended family, thinking their medical nightmare was over.
“I was so happy to be home enjoying my newborn baby and suddenly I felt like I couldn’t breathe again,” Elliott said.
Within 48 hours, and in the midst of a highly infectious omicron wave of COVID-19 that saw hospitals stretched to their limits, Elliott was in an ambulance headed back to Mercy.
“When she got to the ER, her oxygen levels, which should be 92% or more, were at 45%, which I truly didn’t know was possible for someone who was still awake and talking,” Strebel said.
After an initial assessment, Elliott learned she was being admitted to the intensive care stepdown unit. The care team tried everything possible to keep her off a ventilator, using multiple oxygen delivery systems to help her lungs. After a week, she continued to decline and was moved to the intensive care unit for closer monitoring.
“She had a horrible cough, and the work she was putting into breathing prior to intubation was so great, she lost thirty pounds in a couple weeks,” Dr. Strebel said. “She couldn’t eat because she couldn’t do anything but work to breathe.”
After a few weeks, she started to improve, and her caregivers considered a move back to the stepdown unit. Her nurse advocated to keep her in the ICU one more night, a decision that likely saved Elliott’s life. That same day, her oxygen levels deteriorated rapidly, and she was intubated and hooked up to a ventilator that would breathe for her.
“Her blood pressure dropped so low, and the nurses immediately jumped in, but everything we tried to do to intervene medically wasn’t working,” said. Dr. Maroun Tawk, medical director of the intensive care unit.
She was too sick and unstable to get the kind of imaging needed for a clear diagnosis, and there was no time to spare. Dr. Tawk knew something else was wrong but only had adrenaline, intuition and years of experience to make instant decisions.
Tawk called Dr. Aaron Graham, interventional radiologist at Mercy, to explain the emergency and ordered a mobile X-ray and echocardiogram immediately to her beside. He had a rapidly declining patient on the verge of death. The images weren’t clear, but his gut said she had a pulmonary embolism blocking blood flow to her heart.
“This was a huge risk,” Tawk said. “We had no idea what we were dealing with or what Dr. Graham would find if she even survived the short trip down the hall to the cath lab, but we had to do something. She was dying.”
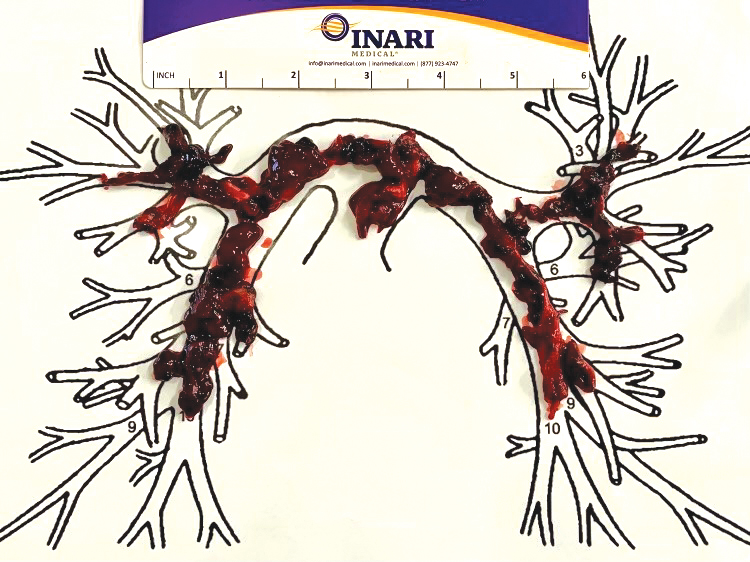
Dr. Graham found a massive bilateral pulmonary embolism unlike anything he and Dr. Tawk had seen before. The clot created a complete obstruction of blood flow in her heart and both lungs. Her family learned she had a 5% chance of surviving the procedure to remove the clots.
“She died on the table,” Dr. Graham said. “I was going in to pull out the clot in her heart, and her heart just stopped beating. The ICU nurses jumped in to start compressions, but I yelled “Stop!” I knew I had to get the blood moving again. As soon as I was able to get a portion of that clot out, her heart started right back up, and it was a mad dash to pull out as much of the remaining clot in her heart and lungs as possible.”













