New findings from the Oklahoma Medical Research Foundation will help doctors better predict an individual’s risk of developing an autoimmune disease and to understand how immune systems of some family members prevent autoimmune diseases.
Autoimmune diseases are conditions in which the immune system becomes unbalanced and turns on the body instead of protecting it. Many of these illnesses strike women at much higher rates than men.
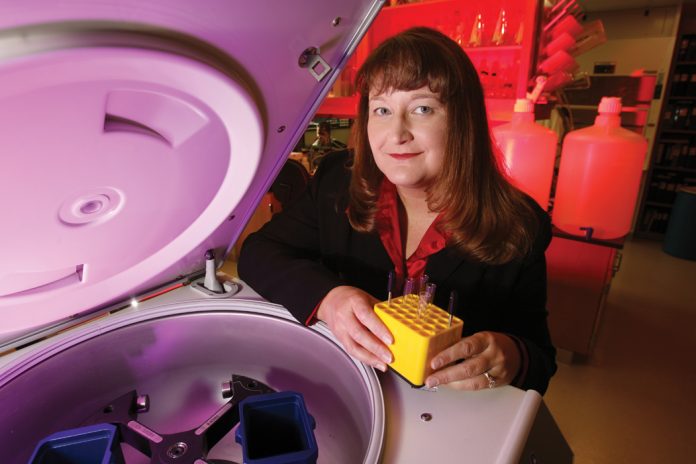
OMRF scientists led by Judith James, M.D., Ph.D., partnered with researchers from the University of Colorado and Benaroya Research Institute, to reveal that healthy people at risk of developing one autoimmune disease also may have autoantibodies typically associated with another autoimmune condition.
“We brought together groups that study different autoimmune diseases to ask: ‘Where does autoimmunity start?’” said James, OMRF’s Vice President of Clinical Affairs and Chair of the Arthritis and Clinical Immunology Research Program.
James said the research looked at samples from large collections of lupus, rheumatoid arthritis and type 1 diabetes patients, and their family members, with the goal of identifying some of the first things that go wrong in autoimmunity.
“If you’re in a family with a person who has RA, do you have blood markers that only look like rheumatoid arthritis, or could they also look like lupus or type 1 diabetes?” said James. “It’s important to understand if individuals start with abnormal immune responses to many different factors which cross autoimmune diseases or if they just start with markers specific to one disease.”
Findings revealed lupus family members in particular were more likely to have antibodies seen in patients who go on to develop lupus, but some also had antibodies for RA and other autoimmune diseases present.
“We’ve found that you are probably more likely to have blood markers of autoimmunity if you’re in a family with someone who has lupus or RA, even though most of the time you will not develop an autoimmune disease,” she said.
This knowledge will help further disease prevention trials like two currently underway at OMRF for lupus and rheumatoid arthritis.
“Instead of trying to figure out the best way to treat patients who already have an established disease, which often has already resulted in irreparable damage, we want to prevent the diseases from occurring long before damage is done,” said James, who also holds the Lou C. Kerr Chair in Biomedical Research.
If they can see blood markers at early time points, clinicians might think about different ways to treat patients. “We may need to think about medications treating broader pre-clinical autoimmunity in general as opposed to targeting a specific disease,” she said.
The findings were published in the journal EBioMedicine, and the research was funded by the National Institute of Allergy and Infectious Diseases, part of the National Institutes of Health.
For more information about the lupus prevention study, known as the SMILE trial, or the StopRA rheumatoid arthritis prevention study, please call (405) 271-7745 or email [email protected].